I thought it would be useful to post a summary of a recent presentation I gave about myositis to the Rheumatology Dept at Newcastle. I hope you find this of some use. Don't hesitate to post comments if you have any feedback or questions.
Click on the below link to access my presentation in PDF format
Inflammatory myopathy: useful hints to help clinical judgement in diagnostics and treatment course
Also, if you want to learn more about MYONET, the international myositis network for scientists and clinicians, click here
I try to provide useful updates about all things medical (and the odd non-medical thing) on my twitter feed @drhectorchinoy
Hopefully more useful presentations to follow in the coming weeks
Cheers
Hector
16th Apr 2016
Rheum blog
Saturday, 16 April 2016
Friday, 7 November 2014
To choose Occam or Hickum, how astute are your specialist skills?
William of Ockham (/ˈɒkəm/; also Occam; c. 1287 – 1347)
I saw a patient the other day that got me thinking. The patient in question had been seen by a number of specialists over the years and there was a family history of rheumatoid arthritis and fibromyalgia. The rheumatoid factor was negative, but as you are aware that does not exclude a diagnosis of rheumatoid arthritis. They were suffering with a constellation of symptoms affecting her neck, shoulders, elbows, wrists, knees and toes. Inflammatory markers namely ESR and CRP had proved normal.
Clinical examination revealed some tension around the neck area, signs in the shoulder consistent with rotator cuff tendinopathy, tennis elbow, De Quervain's tenosynovitis in the long extensor tendons of the thumb, signs of an infrapatellar bursitis and pain in the intermetatarsal space consistent with either an intermetatarsal bursitis or Morton's neuroma.
Now it would be easy to combine these symptoms together and come up with chronic widespread pain consistent with fibromyalgia syndrome, or a possible psoriatic pattern of arthropathy. The latter had been suspected and mooted to the patient by her general practitioner, but then rather unhelpfully reiterated by subsequent specialists. Therein lies the danger of using Occam's razor in diagnostics. Beware of the stage in training where one may “know a little about a lot”; when there is an awareness of diagnostic syndromes, but less of a deeper appreciation of the subtleties that may be involved in making a confident, specialist and accurate diagnosis, in other words pigeon-holing patients into a convenient diagnosis. In fact a greater challenge is to go against what previous physicians may have suspected or what the patient is worried about. This is then going towards the making the more difficult call of Hickam's dictum, where a constellation of symptoms can in fact be discreet. The principle commonly stated is that "Patients can have as many diseases as they damn well please” - as you may suspect Hickam, lived west of the Atlantic!
The ancillary investigations affirmed what I thought was going on clinically, i.e. there was no evidence of an underlying inflammatory arthropathy, I was then able to confirm my initial clinical call and put the patient on the correct treatment pathway. I think the patient was relieved, more so being given a clear message that this was not a unifying diagnosis and then receiving the correct treatments. At the same time, they questioned why they had been previously told they had inflammatory arthritis. Patients believe what they are told and what they read on the web: w+x+y+z does not always equal lupus even though you can somehow force symptoms to suit a criteria. Labelling patients with a syndrome is not helpful when they don’t actually have one! Unlabelling patients who have an incorrect syndrome is even harder. To be told that you don’t have lupus after living with the diagnosis for years is…I dread to think.
The question that I’m putting to any budding specialists in your respective fields is: do you have what it takes to question Occam and embrace Hickam? When an ancillary specialty refers to you, e.g. orthopaedics referring to rheumatology, and asks the question whether this could be e.g. polymyalgia rheumatic, rheumatoid arthritis etc, have the confidence in your convictions to disprove Occam. At the same time, you still require the basis of core specialist knowledge to be aware of more unusual syndromes to apply the razor (sub-specialism - I’ll save that for another day!). Do you now know a “lot about a little” - if so then maybe you have some of the tools required to be a specialist! Maybe my life will then become easier in the future and I can stop re-classifying patients with lupus into ANA positive tennis elbow!
By the way, if you know anyone in the UK/EU who may be interested in carrying out a PhD with our team, feel free to enquire further here or contact me on hector.chinoy@manchester.ac.uk. The title of the project is "Bioinformatic and functional characterization of genetic variants associated with autoimmune idiopathic inflammatory myopathy".
By the way, if you know anyone in the UK/EU who may be interested in carrying out a PhD with our team, feel free to enquire further here or contact me on hector.chinoy@manchester.ac.uk. The title of the project is "Bioinformatic and functional characterization of genetic variants associated with autoimmune idiopathic inflammatory myopathy".
Friday, 11 July 2014
The raison d'être of academia
Things never quite work out the way you want them to in academia (or when you play Germany). Finger clicking or reputation alone doesn't seem to do the trick. It's hard work, sheer doggedness, never accepting your fate, turning a rejection around to a positive, time management, keeping your staff engaged. And keeping the family happy at home! Why do we do it - it enriches us, makes life so much more interesting, and somewhere somehow you'd like to thing you are making a difference. Always useful to remind ourselves about our raison d'être when the chips are down!
Hector Chinoy PhD FRCP
www.inflammation-repair.manchester.ac.uk/staff/HectorChinoy/
www.twitter.com/drhectorchinoy
Tuesday, 8 July 2014
Use of the term "Doctor" - please be open and upfront to your patients
Is it fair on patients that non-medical practitioners can use the title Dr without opening stating they are not a physician?
I had a consultation recently where a patient had seen a chiropractor who used the title Dr. The patient assumed that the chiropractor was a doctor and it is not clear on the practitioner's website at all about this - I can't find any qualifications. I realise that chiropractors can use the term Dr, I'm fine about this, but please be upfront to your patients! The patient then asked me if I was a doctor....got my back up slightly, but actually a fair enough question, who is the patient supposed to believe now that he has this revelation to deal with? I may as well not have bothered with my 5 yrs training for MBBS and 3 years for a PhD! Oh, and my BMedSci, MSc and MRCP. And my 18 years in the NHS.
Patients don't know that they may be seeing practitioners who are not actual medical doctors. It's not mentioned and an assumption is then made. Now I don't have a problem with patients seeing osteopaths or chiropractors; I think they have something valuable to providing an angle that we don't offer as rheumatologists. They can teach us a lot about aspects of musculoskeletal care we are not very good at. What I do mind about is when the boundaries become blurred and it is not made absolutely clear to patients who they are dealing with. Years of medical training allows us to create multiple iterations of possible diagnoses, associations and possible drug interactions during a consultation, so that when the patient is eventually referred on for more targeted treatments the relevant healthcare professional can target appropriate treatment on the back of an accurate diagnosis and more importantly exclusion of other stuff. If something goes wrong or a complication occurs as a result of treatment who is it that has the medical indemnity to cover themselves?-- it's the physician who pays large amounts for yearly cover.
I realise that optometrists, veterinarians, chiropractors can refer to themselves as doctors which I fully accept, but what I would request is that they clearly state that they are a doctor of their relevant specialty and not medicine. State what your qualifications are and make sure that this is visible to your patients on your stationary, website and consulting rooms.
Dr Hector Chinoy
BMBS PhD FRCP MSc BMedSci
I had a consultation recently where a patient had seen a chiropractor who used the title Dr. The patient assumed that the chiropractor was a doctor and it is not clear on the practitioner's website at all about this - I can't find any qualifications. I realise that chiropractors can use the term Dr, I'm fine about this, but please be upfront to your patients! The patient then asked me if I was a doctor....got my back up slightly, but actually a fair enough question, who is the patient supposed to believe now that he has this revelation to deal with? I may as well not have bothered with my 5 yrs training for MBBS and 3 years for a PhD! Oh, and my BMedSci, MSc and MRCP. And my 18 years in the NHS.
Patients don't know that they may be seeing practitioners who are not actual medical doctors. It's not mentioned and an assumption is then made. Now I don't have a problem with patients seeing osteopaths or chiropractors; I think they have something valuable to providing an angle that we don't offer as rheumatologists. They can teach us a lot about aspects of musculoskeletal care we are not very good at. What I do mind about is when the boundaries become blurred and it is not made absolutely clear to patients who they are dealing with. Years of medical training allows us to create multiple iterations of possible diagnoses, associations and possible drug interactions during a consultation, so that when the patient is eventually referred on for more targeted treatments the relevant healthcare professional can target appropriate treatment on the back of an accurate diagnosis and more importantly exclusion of other stuff. If something goes wrong or a complication occurs as a result of treatment who is it that has the medical indemnity to cover themselves?-- it's the physician who pays large amounts for yearly cover.
I realise that optometrists, veterinarians, chiropractors can refer to themselves as doctors which I fully accept, but what I would request is that they clearly state that they are a doctor of their relevant specialty and not medicine. State what your qualifications are and make sure that this is visible to your patients on your stationary, website and consulting rooms.
Dr Hector Chinoy
BMBS PhD FRCP MSc BMedSci
Thursday, 31 October 2013
Resurrection of the Rheum Blog
Rheum Blog returns
I thought I would resurrect my blog post with some useful
information that I've come across over the last few weeks. This is mainly come
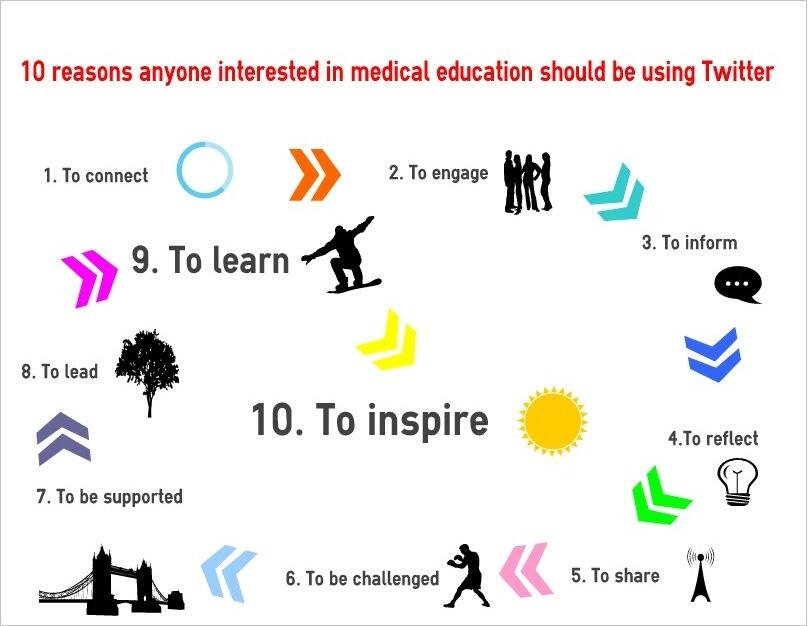
about as I've have started actively using Twitter (follow me @drhectorchinoy, btw Prof Bruce is still ahead of me with followers (@Lupusdoc)!.
I know that there are a few of you skeptical about use of social media and what possible use Twitter could have in terms of clinical medicine and academia. I must say that I otherwise would not have come across some vital information pertaining to updates at the recent ACR conference (eg Biologics or Triple Therapy? The Great Debate at #ACR13), posts about recent advance access publications, articles in the national press relevant to medicine, opinions from key leaders in the field, and useful apps that can make our lives a lot easier when collecting together information. The list goes on and I hope you provide you with a few examples of what I've picked up over the the coming weeks.
Picture courtesy of @KangarooBeach
I know that there are a few of you skeptical about use of social media and what possible use Twitter could have in terms of clinical medicine and academia. I must say that I otherwise would not have come across some vital information pertaining to updates at the recent ACR conference (eg Biologics or Triple Therapy? The Great Debate at #ACR13), posts about recent advance access publications, articles in the national press relevant to medicine, opinions from key leaders in the field, and useful apps that can make our lives a lot easier when collecting together information. The list goes on and I hope you provide you with a few examples of what I've picked up over the the coming weeks.
Referencing software
I've encountered a great piece of free referencing software that would be invaluable for our MSc students. Thank you to Dr Chetan Narshi @Rheumi_ for pointing me in the direction of this. Previously, The University of Manchester has some gone along with either Reference Manager or EndNote – the problem I've encountered with RefMan is that the software costs money for my students outside the university and I have encountered issues when I'm trying to access my lists of references remotely from outside computers – I simply can't do this. Mendeley gets over these problems. It is free to use you can download it to your PC tablet phone etc, and it is web-based. This link provides a useful comparison to other referencing software. You can store 2 GB of data which is more than enough to be getting on with. One of the features that I really like it you can drag-and-drop PDFs into the app and it will effectively turn into a reference for you. Like Reference Manager and EndNote, there is a plug-in that you can use in Word to start creating reference lists.
I've encountered a great piece of free referencing software that would be invaluable for our MSc students. Thank you to Dr Chetan Narshi @Rheumi_ for pointing me in the direction of this. Previously, The University of Manchester has some gone along with either Reference Manager or EndNote – the problem I've encountered with RefMan is that the software costs money for my students outside the university and I have encountered issues when I'm trying to access my lists of references remotely from outside computers – I simply can't do this. Mendeley gets over these problems. It is free to use you can download it to your PC tablet phone etc, and it is web-based. This link provides a useful comparison to other referencing software. You can store 2 GB of data which is more than enough to be getting on with. One of the features that I really like it you can drag-and-drop PDFs into the app and it will effectively turn into a reference for you. Like Reference Manager and EndNote, there is a plug-in that you can use in Word to start creating reference lists.
PubMed Commons
An astonishing development in open access is PubMed Commons. This is really quite groundbreaking – we are all familiar with using
PubMed for looking up sources of evidence and research and that up until now
we've not been able to comment openly about published data. There is no
facility, albeit on a pilot basis for signed up members of department to
comment on their own or, other peoples' manuscripts, and also invite authors of
manuscripts to comment on their publications. You can read about how things
took off in this excellent article by @hildabast.
Ok, promise to post again sooner than the gap from the last post! I'll leave you with this.
Ok, promise to post again sooner than the gap from the last post! I'll leave you with this.
Image courtesy of Maria Popova, click name for full posting
Monday, 21 January 2013
University Faculty Away Day in Manchester
Faculty Away Day
At the Faculty of Medical and Human Sciences University Away Day today at the Manchester Convention Centre, there was a talk from Tony Freemont, the head of undergraduate education at The University of Manchester. He discussed the new technologies that have been introduced to medical students. All students are being supplied with iPads now, which has transformed the delivery of education. Students now no longer have to attend lectures, and students around the world can partake in a global health unit. Whereas previously, students had to attend courses to get to grips with technologies that the university delivers, whereas this is now the opposite, and students are asking the university why they don't have particular technologies available for them to integrate apps and other novel methods of learning into their courses. Tony has an excellent blog which is well worth following to keep up to date with Manchester Medical School Matters: Prof Freemont's Med School Matters blog

Grant Applications
The number and value of research applications coming through nationally has gone down in 2008-10, but in the last year the proportion of applications has gone up by 64.9%. There's an integrated research support service for academics in the research deanery, run by Graham Cadwallader.
You can keep in contact with the research deanery via their twitter feed on @RD_UOM
By the way I also have a twitter feed which I try to keep updated with interesting new in press publications on @drhectorchinoy
There was also an interesting dance by the dean, Ian Jacobs, Faculty Dean with some of the other senior members of staff! I'll send you a link if you are interested in seeing this - not brave enough to post on Youtube!
Branding
The University of Manchester has a new(ish) logo which you should all use for any future presentations. The link is here
Thursday, 3 January 2013
New Year
Dear all
Welcome, as Programme Director of the Rheumatology MSc programme at The University of Manchester, I thought it would be useful to start off a blog to improve communications with past, present and future students on our course.
I'll try to use this blog to keep you updated about developments in the Rheumatology MSc course and anything else interesting I come across. Please use it to post (constructive) comments and feedback.
The main things I'm working on at the moment are trying to freeze fees for the coming year, and introducing new technologies into the course.
Best Wishes for the New Year
Hector Chinoy
Welcome, as Programme Director of the Rheumatology MSc programme at The University of Manchester, I thought it would be useful to start off a blog to improve communications with past, present and future students on our course.
I'll try to use this blog to keep you updated about developments in the Rheumatology MSc course and anything else interesting I come across. Please use it to post (constructive) comments and feedback.
The main things I'm working on at the moment are trying to freeze fees for the coming year, and introducing new technologies into the course.
Best Wishes for the New Year
Hector Chinoy
Subscribe to:
Comments (Atom)